If you are a woman experiencing migraines it is almost certain that like me, you have noticed some sort of correlation between your cycle and your migraines. Although chronic migraine may make it difficult to identify estrogen cycle fluctuations as your trigger due to migraine frequency. So what about our cycles makes us susceptible to migraines at specific times versus others? There have been numerous studies suggesting a connection to estrogen.
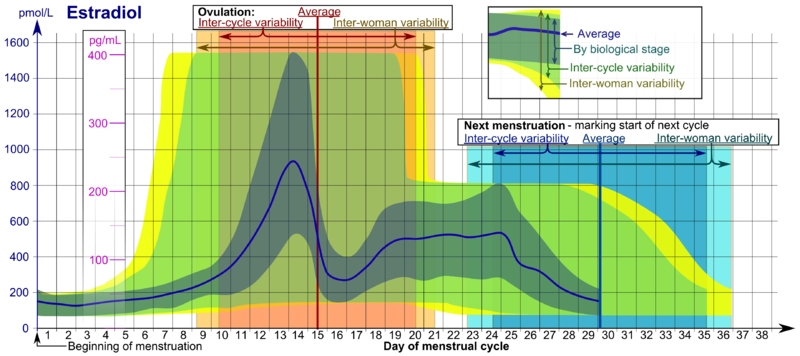
If we take a look specifically at estrogen during a female cycle, this is what happens:
1. Menstruation: estrogen typically measures at a low of <50 pg/ml (first 7 days of graph)
2. Follicular development: estrogen increases during follicular development and peaks at about 200 pg/ml (peak pictured in graph)
3. Ovulation: estrogen drops briefly during ovulation (around day 16 pictured in graph)
4. Luteal phase: estrogen rises again for a second peak (roughly days 20-24 pictured in graph)
5. End of Luteal phase: estrogen level drop to their menstrual levels (assuming we aren't pregnant)
For me personally I tend to "struggle" around (1.) menstruation and (3.) ovulation. These are both times in the female cycle where estrogen is dropping. Estrogen related migraines usually are due to a drop in circulating estrogen after exposure to higher levels of estrogen for a few days (this is referred to as estrogen priming). This "priming" happens naturally at the beginning of menstruation or immediately after giving birth (and lucky me, after delivering both of my beautiful children I had a tremendous migraine).
Other instances that can cause a change in estrogen levels include:
1. A purposeful withdrawal from an estrogen containing product (birth control) during the hormone-free week or interruptions in estrogen therapy.
2. Unintentional withdrawal from estrogen by missing doses of pills or as a result of drug interactions that may reduce estrogen availability.
This made me wonder exactly how and why does this drop in estrogen trigger a migraine?
While investigating I came across a connection between estrogen and serotonin. Estrogen may also impact migraines by affecting other chemical mediators like nitric oxide, magnesium, and prostaglandins which help keep balance between
excitatory and inhibitory neurotransmission. However I find the estrogen-serotonin connection particularly interesting. If you are familiar with migraine medications then you know that one of the most effective abortive medications for migraine are a class of drugs called triptans. These drugs are serotonin receptor agonists (meaning they bind to the specific receptors in the brain that bind to serotonin). They work because once they bind that receptor on cranial vessels they cause vasoconstriction (shrinking of the vessels) as well as a decrease the release of a neuropeptide that causes inflammation. Estrogen impacts the central nervous systems in a number of ways. When estrogen levels drop, serotonin levels fall and there is also an increase in the rate of serotonin elimination. With the drop in serotonin two things happen that could impact a migraine: a release of calcitonin gene-related peptide (which is a potent vasodilator or vessel expander that is produced in both peripheral and central neurons) and a release of substance P (which is associated with pain and inflammation) from trigeminal nerves. To sum it all up, this drop in estrogen has begun a process that leads to vasodilation of cranial blood vessels and pain and inflammation via the trigeminal nerve.
**My graph of the female hormones during cycle was made available thanks to Wikipedia
If we take a look specifically at estrogen during a female cycle, this is what happens:
1. Menstruation: estrogen typically measures at a low of <50 pg/ml (first 7 days of graph)
2. Follicular development: estrogen increases during follicular development and peaks at about 200 pg/ml (peak pictured in graph)
3. Ovulation: estrogen drops briefly during ovulation (around day 16 pictured in graph)
4. Luteal phase: estrogen rises again for a second peak (roughly days 20-24 pictured in graph)
5. End of Luteal phase: estrogen level drop to their menstrual levels (assuming we aren't pregnant)
For me personally I tend to "struggle" around (1.) menstruation and (3.) ovulation. These are both times in the female cycle where estrogen is dropping. Estrogen related migraines usually are due to a drop in circulating estrogen after exposure to higher levels of estrogen for a few days (this is referred to as estrogen priming). This "priming" happens naturally at the beginning of menstruation or immediately after giving birth (and lucky me, after delivering both of my beautiful children I had a tremendous migraine).
Other instances that can cause a change in estrogen levels include:
1. A purposeful withdrawal from an estrogen containing product (birth control) during the hormone-free week or interruptions in estrogen therapy.
2. Unintentional withdrawal from estrogen by missing doses of pills or as a result of drug interactions that may reduce estrogen availability.
This made me wonder exactly how and why does this drop in estrogen trigger a migraine?
While investigating I came across a connection between estrogen and serotonin. Estrogen may also impact migraines by affecting other chemical mediators like nitric oxide, magnesium, and prostaglandins which help keep balance between
excitatory and inhibitory neurotransmission. However I find the estrogen-serotonin connection particularly interesting. If you are familiar with migraine medications then you know that one of the most effective abortive medications for migraine are a class of drugs called triptans. These drugs are serotonin receptor agonists (meaning they bind to the specific receptors in the brain that bind to serotonin). They work because once they bind that receptor on cranial vessels they cause vasoconstriction (shrinking of the vessels) as well as a decrease the release of a neuropeptide that causes inflammation. Estrogen impacts the central nervous systems in a number of ways. When estrogen levels drop, serotonin levels fall and there is also an increase in the rate of serotonin elimination. With the drop in serotonin two things happen that could impact a migraine: a release of calcitonin gene-related peptide (which is a potent vasodilator or vessel expander that is produced in both peripheral and central neurons) and a release of substance P (which is associated with pain and inflammation) from trigeminal nerves. To sum it all up, this drop in estrogen has begun a process that leads to vasodilation of cranial blood vessels and pain and inflammation via the trigeminal nerve.
**My graph of the female hormones during cycle was made available thanks to Wikipedia
















 RSS Feed
RSS Feed
